What is ccf in medical terms – Embarking on an exploration of congestive cardiac failure (CCF), this article unravels its complexities with clarity and precision, guiding readers through its definition, types, diagnosis, management, and prognosis.
CCF, a condition where the heart struggles to pump blood effectively, affects millions worldwide. This comprehensive guide delves into the intricacies of CCF, empowering readers with knowledge and understanding.
Congestive Cardiac Failure (CCF)
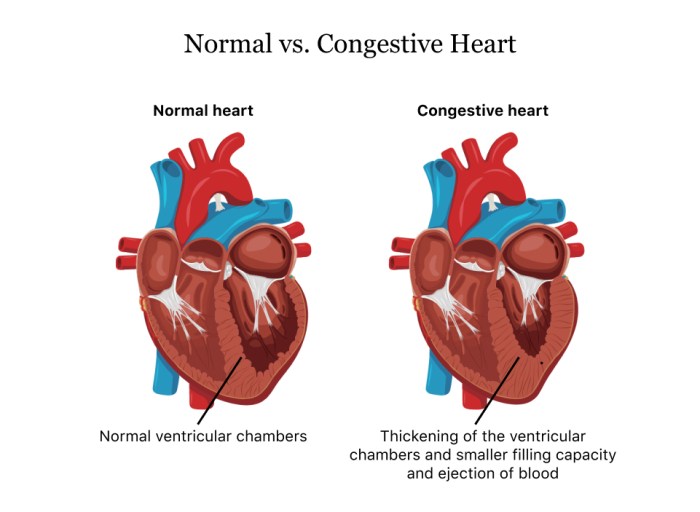
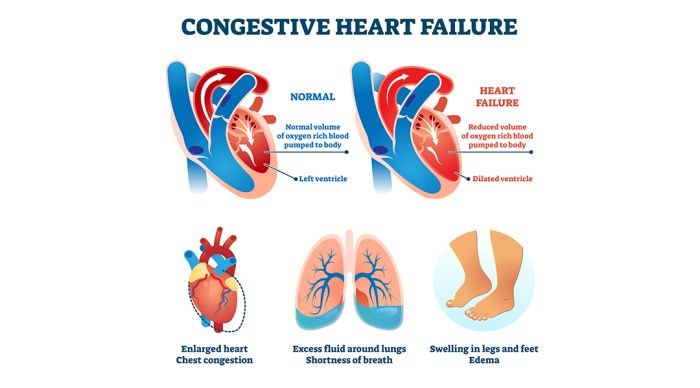
Congestive cardiac failure (CCF) is a condition in which the heart is unable to pump enough blood to meet the body’s needs. This can lead to a buildup of fluid in the body, which can cause swelling in the legs, ankles, and feet, as well as shortness of breath and fatigue.
CCF is a serious condition that can lead to death if not treated. However, with proper treatment, most people with CCF can live long and full lives.
Pathophysiology
The pathophysiology of CCF is complex and involves a number of factors. However, the most common cause of CCF is coronary artery disease (CAD). CAD is a condition in which the arteries that supply blood to the heart become narrowed or blocked by plaque.
This can lead to a heart attack, which can damage the heart muscle and lead to CCF.
Other causes of CCF include:
- High blood pressure
- Diabetes
- Obesity
- Smoking
- Alcohol abuse
- Certain medications
- Viral infections
- Genetic disorders
Clinical Manifestations, What is ccf in medical terms
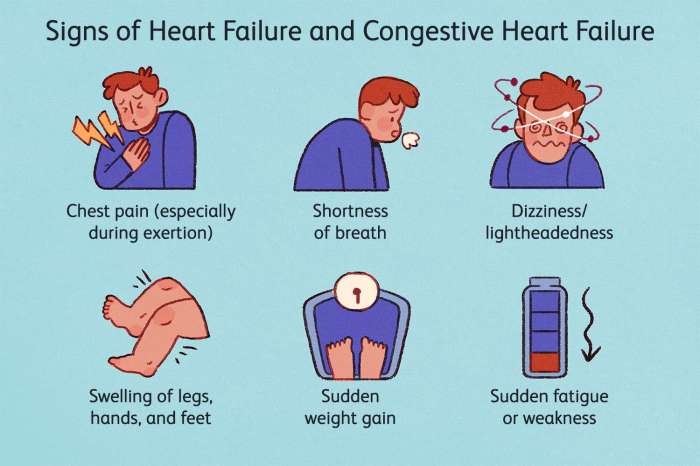
The clinical manifestations of CCF can vary depending on the severity of the condition. However, some of the most common symptoms include:
- Shortness of breath
- Fatigue
- Swelling in the legs, ankles, and feet
- Rapid or irregular heartbeat
- Chest pain
- Lightheadedness or dizziness
- Confusion
- Nausea or vomiting
Types of Congestive Cardiac Failure
Congestive cardiac failure (CCF) is a complex condition that can affect different parts of the heart. There are three main types of CCF: left-sided, right-sided, and biventricular failure.
Each type of CCF has its own unique causes, symptoms, and treatment options.
Left-sided CCF
Left-sided CCF occurs when the left ventricle of the heart is unable to pump blood effectively. This can be caused by a variety of factors, including:
- Coronary artery disease
- Heart attack
- High blood pressure
- Diabetes
- Cardiomyopathy
Symptoms of left-sided CCF include:
- Shortness of breath
- Fatigue
- Swelling in the legs, ankles, and feet
- Chest pain
- Coughing up blood
Treatment for left-sided CCF includes medications to improve heart function, diuretics to reduce fluid retention, and lifestyle changes such as diet and exercise.
Right-sided CCF
Right-sided CCF occurs when the right ventricle of the heart is unable to pump blood effectively. This can be caused by a variety of factors, including:
- Pulmonary embolism
- Chronic obstructive pulmonary disease (COPD)
- Pulmonary hypertension
- Heart failure
- Coronary artery disease
Symptoms of right-sided CCF include:
- Swelling in the legs, ankles, and feet
- Abdominal pain
- Nausea and vomiting
- Fatigue
- Jaundice
Treatment for right-sided CCF includes medications to improve heart function, diuretics to reduce fluid retention, and lifestyle changes such as diet and exercise.
Biventricular CCF
Biventricular CCF occurs when both the left and right ventricles of the heart are unable to pump blood effectively. This is the most severe type of CCF and can be fatal if not treated promptly.
Symptoms of biventricular CCF include:
- Shortness of breath
- Fatigue
- Swelling in the legs, ankles, and feet
- Chest pain
- Coughing up blood
- Nausea and vomiting
- Jaundice
Treatment for biventricular CCF includes medications to improve heart function, diuretics to reduce fluid retention, and lifestyle changes such as diet and exercise. In some cases, a heart transplant may be necessary.
Diagnosis of Congestive Cardiac Failure: What Is Ccf In Medical Terms
Congestive cardiac failure (CCF) can be challenging to diagnose, as its symptoms often overlap with other conditions. A comprehensive evaluation involving physical examination, medical history, laboratory tests, and imaging techniques is crucial for accurate diagnosis.
Physical Examination
Physical examination provides valuable clues about CCF. Signs of fluid retention, such as edema in the legs, ankles, and feet, indicate possible heart failure. Auscultation of the heart may reveal abnormal heart sounds, such as a third heart sound (S3) or a fourth heart sound (S4), which can suggest impaired ventricular function.
Medical History
A detailed medical history can help identify potential risk factors for CCF, such as hypertension, diabetes, coronary artery disease, or a family history of heart failure. Symptoms reported by the patient, such as shortness of breath, fatigue, and exercise intolerance, can provide further insights into the severity of CCF.
Laboratory Tests
Blood tests can detect elevated levels of certain biomarkers, such as B-type natriuretic peptide (BNP) and N-terminal pro-BNP (NT-proBNP), which are indicators of heart failure. Other tests, such as a complete blood count and electrolyte panel, can help rule out other underlying conditions.
Imaging Techniques
Imaging techniques play a vital role in confirming the diagnosis of CCF. Echocardiography, an ultrasound of the heart, can assess the size, shape, and function of the heart chambers, valves, and pericardium. Chest X-rays can reveal signs of pulmonary edema, an accumulation of fluid in the lungs, which is a common manifestation of CCF.
Other imaging techniques, such as cardiac magnetic resonance imaging (MRI) or computed tomography (CT), may be used in specific cases to further evaluate the heart and its structures.
Management of Congestive Cardiac Failure
The management of Congestive Cardiac Failure (CCF) involves a combination of treatment options and lifestyle modifications aimed at improving the heart’s function, reducing symptoms, and preventing complications. Treatment typically includes medications, lifestyle changes, and in some cases, surgery or other procedures.
Medications
Medications play a crucial role in managing CCF. Diuretics, such as furosemide and spironolactone, help reduce fluid retention and improve symptoms of fluid overload. ACE inhibitors, such as captopril and lisinopril, and beta-blockers, such as metoprolol and carvedilol, work to reduce the heart’s workload and improve its pumping efficiency.
Lifestyle Modifications
Lifestyle modifications can significantly improve outcomes in CCF patients. A healthy diet, regular exercise, and smoking cessation are essential components of CCF management. A low-sodium diet can help reduce fluid retention, while regular exercise strengthens the heart and improves its function.
Smoking cessation is crucial as it reduces the risk of further heart damage and improves overall health.
Prognosis and Complications of Congestive Cardiac Failure
Congestive cardiac failure (CCF) is a serious condition that can lead to a variety of complications and even death. The prognosis for patients with CCF depends on the severity of the condition, the underlying cause, and the patient’s overall health.
Patients with mild CCF may live for many years with few symptoms. However, as the condition progresses, the symptoms can become more severe and the prognosis worsens. Patients with severe CCF may only live for a few years.
Complications
CCF can lead to a number of complications, including:
- Pulmonary edema:This is a condition in which fluid builds up in the lungs, making it difficult to breathe.
- Arrhythmias:These are abnormal heart rhythms that can be dangerous.
- Renal failure:This is a condition in which the kidneys are unable to function properly.
- Liver failure:This is a condition in which the liver is unable to function properly.
- Death:CCF is a leading cause of death in the United States.
Importance of Monitoring and Follow-Up Care
Monitoring and follow-up care are essential for patients with CCF. This care can help to prevent complications and improve outcomes. Patients with CCF should see their doctor regularly for checkups and to make sure that their medications are working properly.
Final Review
In conclusion, CCF is a multifaceted condition with varying presentations and management strategies. Understanding its complexities is crucial for healthcare professionals and patients alike, as it empowers informed decision-making and improves outcomes.
Through continuous research and advancements in treatment, the future of CCF management holds promise for better patient care and improved quality of life.
Top FAQs
What are the common symptoms of CCF?
Shortness of breath, fatigue, swelling in the legs and feet, and coughing up pink or blood-tinged sputum.
What are the different types of CCF?
Left-sided CCF, right-sided CCF, and biventricular CCF.
How is CCF diagnosed?
Through a combination of physical examination, medical history, laboratory tests, and imaging techniques such as echocardiography and chest X-rays.
What are the treatment options for CCF?
Medications (diuretics, ACE inhibitors, beta-blockers), lifestyle modifications (diet, exercise, smoking cessation), and in some cases, surgical interventions.